Symptoms: From Joint Pain to Systemic Effects
Rheumatoid arthritis arises from chronic inflammation of the synovium, the tissue lining the joints, which can damage cartilage, erode bone, and ultimately lead to joint destruction. In severe cases, it may cause significant functional impairment. The condition affects women three to five times more frequently than men and can manifest across all age groups.
Early symptoms, often called prodromal signs, include fatigue, loss of appetite, general weakness, and vague muscle or joint pain that may persist for weeks. As the disease progresses, synovitis develops, causing joint swelling and fluid accumulation. Affected areas—commonly the fingers, wrists, shoulders, elbows, ankles, and knees—typically exhibit symmetrical pain and swelling. A hallmark feature is morning stiffness, where joints feel rigid upon waking and may take more than an hour to loosen—sometimes described medically as ‘gelling.'

Diagnosis: A Multi-Faceted Approach
Diagnosing RA involves a scoring system based on four criteria: joint involvement, blood tests, acute-phase reactant levels, and symptom duration. A total score of 6 or higher confirms the diagnosis.
- Joint Involvement: Joint involvement is scored by the number and type of affected joints: one large joint scores 0, 2–10 large joints score 1, 1–3 small joints score 2, 4–10 small joints score 3, and more than 10 joints (including at least one small joint) score 5.
- Blood Tests: Tests for rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies determine seropositivity. Negative results score 0 points, weakly positive (below three times the upper limit of normal) scores 2 points, and strongly positive (three times or more above the limit) scores 3 points.
- Acute-Phase Reactants: Elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) levels add 1 point.
- Symptom Duration: Symptoms persisting for six weeks or longer add 1 point.
Treatment and Management: Aiming for Remission
RA treatment primarily focuses on pharmacotherapy to control inflammation, relieve symptoms, and slow joint damage. Although a cure remains elusive, current strategies aim for achieving and maintaining remission.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation and pain but may cause gastrointestinal side effects, often requiring co-prescription of protective agents. Corticosteroids provide rapid relief during acute phases but are advised only at low doses and for short-term use, generally limited to within six months, to minimize side effects. Neither NSAIDs nor corticosteroids halt disease progression.
Dr. Lee emphasizes the role of disease-modifying antirheumatic drugs (DMARDs): “DMARDs act on immune pathways to suppress inflammation, alleviate symptoms, and slow disease progression. Early initiation improves outcomes, though effects may take 1–3 months to appear and vary by patient. Combination therapy can enhance effectiveness.” Newer biologic agents and targeted synthetic therapies, which address specific inflammatory pathways or overactive immune cells, are increasingly used worldwide, particularly for patients unresponsive to conventional DMARDs. These therapies allow tailored treatment based on disease severity and progression.
Surgical intervention may be necessary in cases of severe joint destruction or deformity that limits daily function. Because joint damage often affects surrounding structures, thorough consultation with a specialist is essential before surgery.
Non-Pharmacological Management: Balancing Rest and Activity
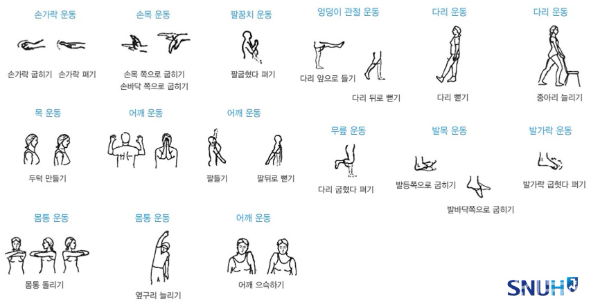
As a chronic condition, RA requires a holistic approach. Dr. Lee notes, “Non-pharmacological treatments like nutrition, physical therapy, exercise, and rest are vital. During acute flares, rest is prioritized to reduce inflammation, but excessive immobility can worsen stiffness. Gentle range-of-motion exercises can help maintain joint mobility without strain.”
Once inflammation subsides, exercise is encouraged to preserve joint function. Patients should aim to perform gentle flexion and extension of affected joints several times daily. Low-impact activities such as walking, swimming, aqua aerobics, cycling, and stretching are recommended, while high-impact exercises and deep squats should be avoided to reduce joint stress.
Dr. Lee concludes, “Though RA is a chronic condition, combining pharmacological and non-pharmacological treatments can prevent joint deformity, reduce pain, and improve quality of life. Understanding prescribed medications and adhering to treatment are critical. While no specific diet is required, maintaining a healthy weight can help reduce joint strain.”
Lim Hye Jung, HEALTH IN NEWS TEAM
press@hinews.co.kr